Every year, as autumn draws to a close, questions about how well the health service is prepared for winter dominate news headlines. This year is no exception, with last week's news headlines highlighting NHS England's warning to GPs and hospitals to expect more cases of flu than usual. This was prompted by the fact that Australia and New Zealand have just experienced their worst outbreak of the influenza virus (flu) for several years, with double the number of cases in 2017, when compared to 2016.1 Co-incidentally, last week our very own public health specialist, Dr Jane Halpin, alerted everyone in our health team to the availability of Deloitte's voucher scheme and urged them to apply for a voucher and make every effort to get the vaccination. We therefore thought we would use this week's blog to enable Jane to explain to us all, especially those staff who visit health organisations on a regular basis, why we should get the vaccination and why it's important to do so every year.
The mutating threat
New strains of flu virus emerge every year, and sweep across the globe from East to West. Thanks to constant mutation, the virus is able to continually mutate into new strains that can pose risks to humans, for this reason some degree of flu outbreak is inevitable each year.
There is often confusion between the flu and the common cold. Both are caused by a virus, and occur roughly during the same months each year (depending on where you are on the planet) and both can share similar symptoms, including: a runny or blocked nose; sore throat and cough.2 However, the flu virus generally causes much more severe symptoms than the cold virus, and can include all the above symptoms, but also: fever and chills; headache; severe tiredness and aching muscles.3
While there is no doubt that seasonal flu can be deadly, especially for the very young and old, as well as those with compromised immune systems, for many people, is not particularly severe because our immune systems are likely to have met and coped with a similar type of flu virus in the previous year or two, and thus know how to fight it. However, from time to time, new strains of virus appear that are very different to those in prior years – meaning there is little existing resistance - leading to higher levels of illness.
There are four types of influenza virus, A, B, C and D.4 Type A represents the greatest threat due to its high tendency for mutation and genetic reassortment5 which can result in a new pandemic strain with severe clinical symptoms and complications, such as chest infections and meningitis.6 These viruses are transmitted from person to person through the inhalation of droplets in the air, and also through touching virally contaminated surfaces and then touching one's nose or mouth. These characteristics coupled with our tendencies to live and work in crowded places, stay indoors during winter, not seek vaccination and not sanitise correctly when illness is suspected, can result in an influenza virus that can have considerable virulence.
Estimates suggest that influenza causes:
- 3 to 5 million cases of severe illness, and 250,000 to 500,000 deaths annually across the globe7
- an average of 600 deaths per year in the UK. However, yearly variation can differ significantly, as an estimated 11,000 people died due to flu related causes in 2013-148. Whilst in the US it is estimated to have caused 57,062 deaths in 2015 (including deaths from pneumonia)9
- an estimated $5.8 billion economic burden to the US10 and a cost of $85 million cost to the Australian healthcare system, annually.11
Warning signs
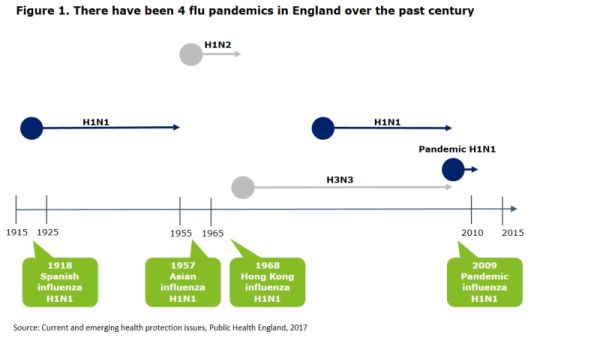
England has experienced four influenza pandemics over the past century (figure 1), The most recent, a mild pandemic in 2009, does not reduce the probability of a future, more significant, pandemic occurring in the near future, as there is an estimated three per cent chance of a significant influenza pandemic each year;12 indeed many public health experts consider that we are overdue another one.13
Taken together, the above factors highlight the need for increasing the awareness and uptake of flu vaccinations amongst the general population in order to lessen the impact on ourselves and the strain on our healthcare services.
The importance of flu vaccinations
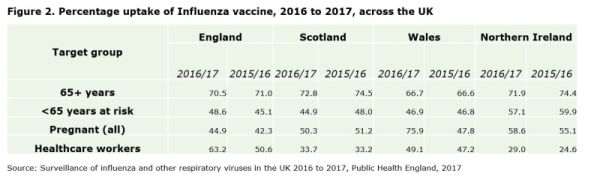
Every year, considerable effort is exerted to predict the strains of influenza that will circulate in the winter months of the coming year and produce an effective vaccination. Therefore it is imperative to be vaccinated against the latest strains every year. Many country's healthcare authorities, including the UK's NHS, provide free vaccinations for at risk groups and healthcare workers. Despite the benefits of free vaccinations certainly outweighing the costs, the uptake of vaccinations in the UK, particularly among healthcare workers, remains low, especially when considering their interactions with at risk groups on a daily basis (figure 2).
Outside of these groups there is also a responsibility amongst the general public to be better aware of the risks the flu poses and to vaccinate accordingly. This should be done not only to protect the general public as a whole, but also to protect at risk groups and to limit the spread of the virus. Though vaccinations are generally not free to those outside of at risk groups, many companies, including Deloitte, offer programmes that encourage employees to acquire vaccinations.
Misconceptions about flu vaccinations
Despite a number of government and employee programmes to promote flu vaccinations, especially amongst at risk groups, vaccination rates in the general public are low; with a number of misconceptions contributing to this, including:
- the flu vaccine gives you the flu -while side effects can occur, the worst effects are often soreness, redness or tenderness where the vaccination was given or a short-lived low grade fever, headache or muscle ache
- serious reactions to the vaccine are common - serious allergic reactions to flu vaccinations are very rare, and if they do occur are noticeable fairly quickly after being given the vaccination. If a reaction is suspected, treatments are available
- a vaccination every year is unnecessary - the influenza virus is highly prone to mutation, and new strains are discovered every year. A vaccination from last year may not offer immunity from a strain discovered this year
- it is too late to get vaccinated - though it is ideal to get vaccinated before the end of October, the flu season is highly variable, and vaccinations just before peak months (December through to March) can make a difference in limiting the spread of the virus.14
Conclusion
Every year thousands of people around the world become seriously ill or die from a viral infection that is preventable. The experience of this year's flu season in Australia is that current strains are more severe than in recent years, with higher rates of infection and higher levels of significant illness – in which case any level of protection will be valuable. As well as protecting ourselves from flu, by getting vaccinated we help reduce the potential to spread flu to more vulnerable people – mainly the elderly and the very young.
This year I would urge everyone not to allow misconceptions and complacency surrounding the flu and flu vaccinations to deter you from getting the jab. Take up government and company offers to get vaccinated or get the vaccine directly from your local pharmacy, as we are we are all at risk from contracting, incubating and spreading influenza this winter.
I have been personally nagging everyone in the health team to get their vaccine, and have asked our Deloitte Clinical Network to do the same with their colleagues! And really for Deloitte employees there is no excuse as you are all eligible for the voucher, albeit you need to get your request in by 29 September!
Footnotes
2 https://onlinedoctor.lloydspharmacy.com/uk/info/difference-between-cold-and-flu
3 Ibid
4 https://www.gov.uk/government/collections/annual-flu-programme
5 http://www.who.int/ith/diseases/si_iAh1n1/en/
6 http://vk.ovg.ox.ac.uk/influenza-flu
7 http://www.who.int/mediacentre/factsheets/fs211/en/
8 http://vk.ovg.ox.ac.uk/influenza-flu
9 https://www.cdc.gov/nchs/fastats/deaths.htm
10 http://content.healthaffairs.org/content/early/2016/10/07/hlthaff.2016.0462.full
11 http://www.isg.org.au/index.php/about-influenza/impact-of-influenza/
13 http://edition.cnn.com/2017/04/07/health/flu-pandemic-sanjay-gupta/index.html
14 https://www.cdc.gov/flu/about/qa/misconceptions.htm
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.
